Description
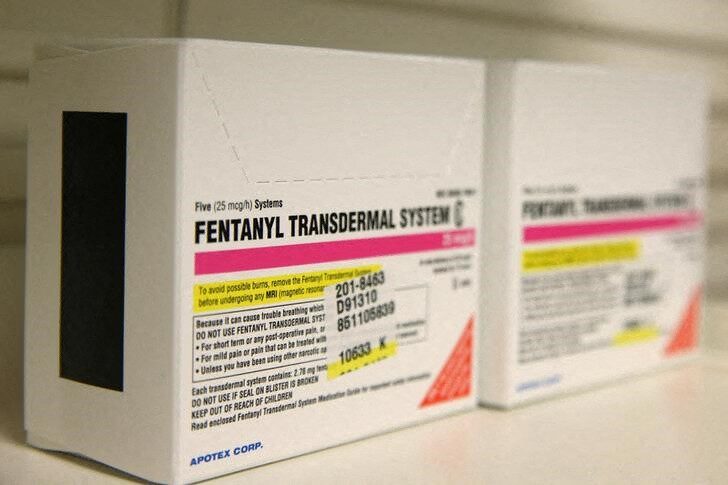
Fentanyl Transdermal System
Buy Fentanyl Transdermal System, commonly called the fentanyl patch, offers powerful relief for chronic pain but raises concerns due to its potency. This opioid medication delivers steady pain control for specific patients, yet its risks demand attention. This blog post explores the fentanyl patch’s uses, benefits, side effects, and regulations, providing clear, factual insights to help readers understand its role in pain management.
What Is the Fentanyl Transdermal System?
The Fentanyl Transdermal System is a skin patch delivering fentanyl, a potent opioid, over 72 hours. Doctors prescribe it for chronic pain in opioid-tolerant patients, such as those with cancer or severe injuries, when other treatments fail. The FDA approved it in 1990, with doses from 12 to 100 micrograms per hour. Fentanyl, 50–100 times stronger than morphine, requires careful dosing. Patients apply patches to clean skin, ensuring steady pain relief. Only licensed pharmacies dispense it with a prescription.
Benefits for Chronic Pain Management
The fentanyl patch provides consistent relief for chronic pain, especially in cancer or post-surgical cases. Studies show it reduces pain intensity for opioid-tolerant patients, improving daily function. Its 72-hour delivery eliminates frequent dosing, offering convenience over pills or injections. Patients report better sleep and mobility when pain is managed. The patch’s controlled release suits long-term needs, avoiding pain spikes. Doctors tailor doses to balance efficacy and safety, making it a valuable option for severe, persistent pain. Close monitoring ensures optimal outcomes for eligible patients.
Risks and Side Effects to Know
The fentanyl patch carries serious risks, including respiratory depression, addiction, and overdose. Common side effects include nausea, constipation, drowsiness, and skin irritation at the patch site. Severe risks, like slowed breathing, can be fatal, especially in non-opioid-tolerant users or if misused. The FDA’s black box warning stresses these dangers, urging medical supervision. X posts highlight misuse concerns, noting accidental overdoses from improper application. Naloxone reverses overdoses if given quickly. Patients must avoid heat sources, like heating pads, which increase fentanyl absorption. Report symptoms immediately to stay safe.
How to Use the Fentanyl Patch Safely
Patients apply the fentanyl patch to clean, dry skin on the chest, back, or arm. Replace it every 72 hours, using a new site to avoid irritation. Never cut patches, as this releases fentanyl too quickly, risking overdose. Start with the lowest effective dose, typically 12 or 25 micrograms per hour, for opioid-tolerant patients. Avoid alcohol or sedatives, which amplify risks. Store patches securely, away from children, as even used patches contain dangerous fentanyl levels. Dispose of used patches by folding and flushing them. Follow doctor’s instructions precisely to ensure safety.
Regulatory Status and Safety Measures
The Fentanyl Transdermal System, a Schedule II controlled substance, requires a prescription and enrollment in the FDA’s TIRF-REMS program for certain fentanyl products. The FDA restricts it to chronic pain in opioid-tolerant patients, not acute or postoperative pain. Pharmacies verify prescriptions, limiting supplies to prevent diversion. X posts warn of illegal sales, emphasizing risks from unregulated sources. Regulations mandate secure storage, as a single patch can harm non-tolerant individuals. Doctors educate patients on proper use and disposal to comply with safety protocols, reducing misuse risks.
Fentanyl Patch and the Opioid Crisis
The fentanyl patch contributes to the opioid crisis, though its medical use is tightly controlled. Illicit fentanyl, not the transdermal system, drives most overdose deaths, with the CDC reporting over 70,000 annual U.S. fatalities from synthetic opioids. Misuse, such as applying multiple patches or using heat, increases risks. X posts note diversion from medical settings, fueling black-market sales. Stricter prescribing guidelines and REMS programs aim to limit abuse. Doctors explore non-opioid pain relief to reduce dependency. Education and monitoring remain key to balancing medical needs and public safety.
Conclusion
The Fentanyl Transdermal System offers effective chronic pain relief for opioid-tolerant patients but demands careful use. Its benefits—steady pain control and convenience—come with risks like respiratory depression. Only use it under medical guidance. Consult your doctor to assess its suitability. Visit the fentanylshop website or trusted sources for details. Stay informed for safe health choices.



Reviews
There are no reviews yet.